Mitigate Pain Clinic – Dr Jeshnu Tople – Pain Management Specialist In Nagpur
Chronic Pelvic Pain
Chronic Pelvic Pain Treatment

What Is Chronic Pelvic Pain?
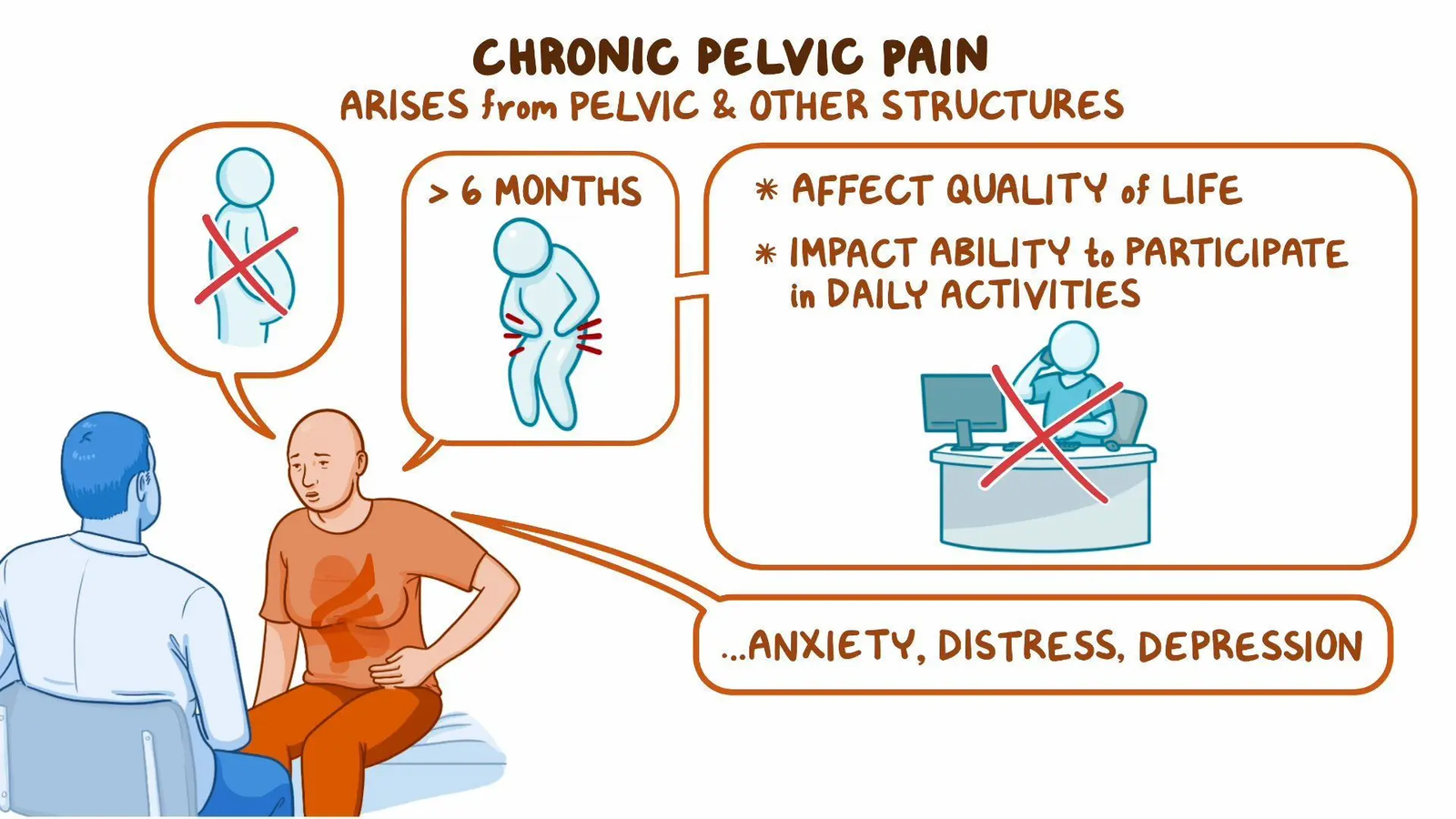
Chronic pelvic pain is a complex condition characterized by pain in the pelvic region that persists for at least six months. The pain can range from mild discomfort to severe, debilitating sensations that interfere with daily activities. While CPP is most commonly associated with women, men can also experience this condition, and its causes are varied and sometimes difficult to pinpoint.
Many people suffering from chronic pelvic pain may also experience:
Pressure or heaviness in the pelvis
Sharp, stabbing pains
Pain during sexual intercourse
Discomfort
Common Causes of Chronic Pelvic Pain
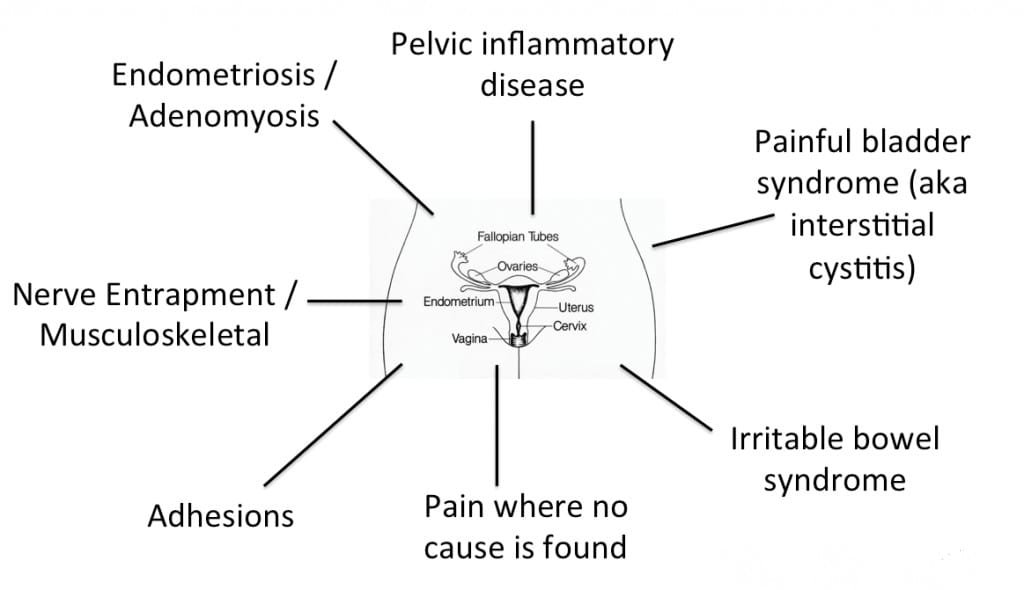
1. Gynecological Conditions
Many women with chronic pelvic pain suffer from gynecological disorders. These conditions include:
● Endometriosis: A condition in which the tissue that normally lines the inside of the uterus grows outside, causing pain and inflammation.
Pelvic Inflammatory Disease (PID): It is inflammation of the reproductive organs.
Uterine Fibroids: Non-cancerous growths in the uterus that can cause significant discomfort.
2. Gastrointestinal Disorders
Chronic pelvic pain can sometimes be linked to gastrointestinal issues such as:
Irritable Bowel Syndrome (IBS): A common disorder that affects the large intestine, leading to cramping, abdominal pain, and bloating.
Inflammatory Bowel Disease (IBD): Chronic inflammation of the gastrointestinal tract, including Crohn’s disease and ulcerative colitis, which can lead to pelvic pain.
3. Urological Problems
Conditions involving the urinary system can also result in chronic pelvic pain:
Interstitial Cystitis: Also known as painful bladder syndrome, this condition causes bladder pressure and pain, often leading to chronic discomfort.
Idiopathic Testicular Pain Idiopathic testicular pain refers to chronic discomfort in the testicles with no identifiable cause after extensive evaluation.
4. Musculoskeletal Issues
Pelvic pain can arise from issues with the muscles, joints, and ligaments in the pelvic region:
Pelvic Floor Dysfunction: Tension or weakness in the pelvic floor muscles can lead to chronic pain and discomfort.
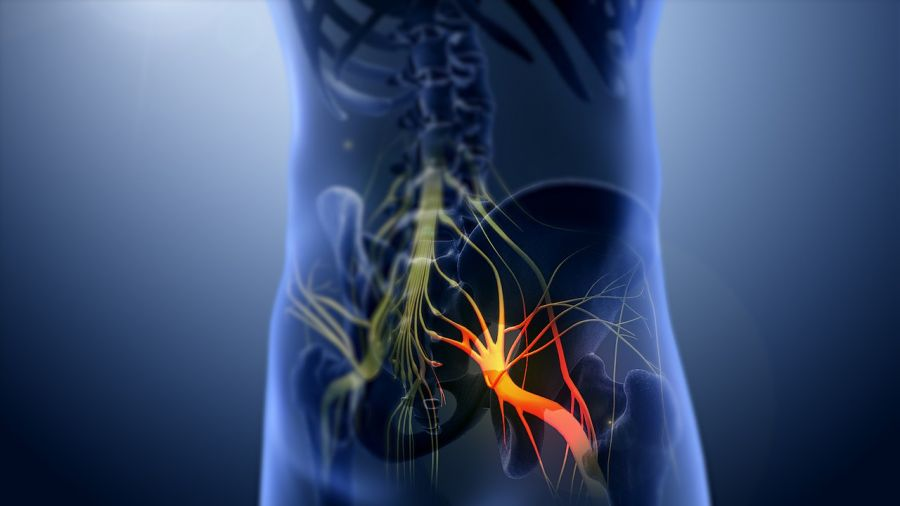
Nerve Entrapment: Compression or irritation of the pelvic nerves, such as the pudendal nerve, can lead to persistent pain.
5. Psychological Factors
Mental health conditions such as anxiety, depression, or a history of trauma can exacerbate chronic pelvic pain. The mind and body are closely linked, and emotional stress can intensify the perception of pain.
Diagnosing Chronic Pelvic Pain
At Mitigate Pain Clinic, our specialists use a comprehensive approach to diagnose chronic pelvic pain. This may include:
Medical History Review: Understanding the patient’s full medical background to identify any underlying conditions.
Physical Examination: A thorough pelvic examination can help identify the source of pain.
Diagnostic Tests: Imaging tests, such as ultrasounds, MRIs, and CT scans, may be used to visualize abnormalities in the pelvic area. Additionally, laboratory tests and diagnostic laparoscopy may be performed to assess gynecological issues.
This meticulous approach ensures that the root cause of your pelvic pain is accurately identified, which is critical for developing an effective treatment plan.
Interventional Pain Management Solutions at Mitigate Pain Clinic
1. Nerve Blocks
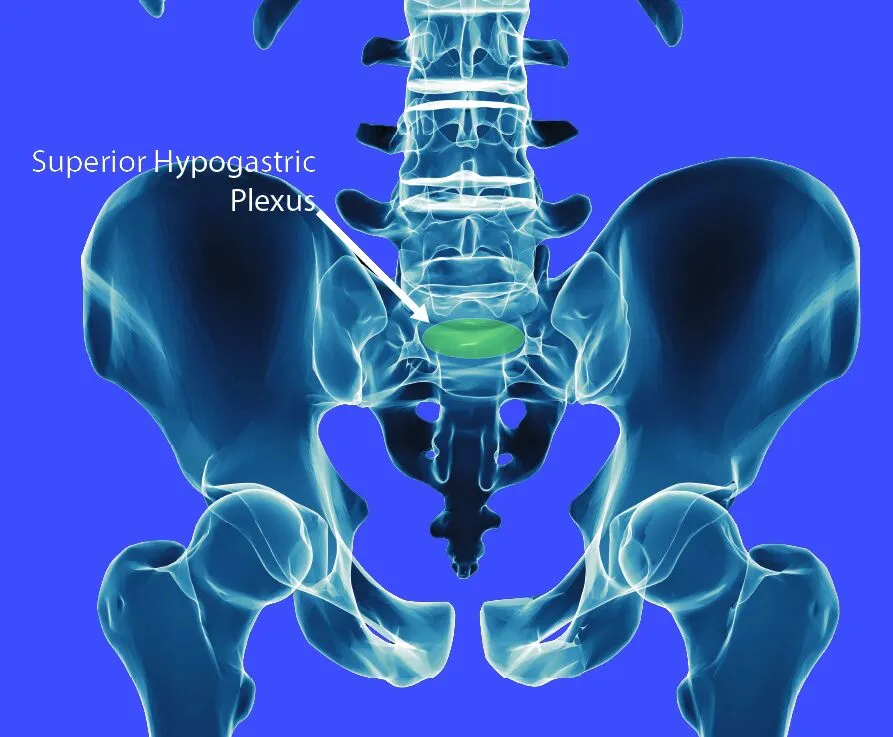
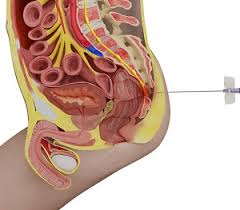
2. Superior Hypogastric Plexus Intervention
3. Ganglion Impar Intervention

4. Spinal Cord Stimulation (SCS)
5. Trigger Point Injections

Benefits of Interventional Pain Management for Chronic Pelvic Pain
Interventional pain management offers several benefits for those suffering from chronic pelvic pain:
Targeted Relief: Unlike systemic treatments like oral medications, interventional procedures focus on the specific nerves and tissues responsible for pain.
Minimally Invasive: Many of the procedures offered at Mitigate Pain Clinic are minimally invasive, resulting in shorter recovery times and fewer risks than surgery.
Improved Quality of Life: By reducing pain and improving mobility, patients can return to their daily activities with minimal disruption.
Personalized Treatment Plans at Mitigate Pain Clinic
At Mitigate Pain Clinic, we understand that chronic pelvic pain affects everyone differently. Our pain management specialist works closely with each patient to develop a personalized treatment plan tailored to their specific condition and lifestyle. Whether your pain is caused by a gynecological issue, a gastrointestinal disorder, or musculoskeletal dysfunction, we have the expertise to help you find relief. The latest medical advancements with compassionate care, ensuring that you receive the best possible treatment for your chronic pelvic pain.
Living with Chronic Pelvic Pain: Tips for Coping
While receiving treatment at Mitigate Pain Clinic, there are several strategies you can adopt to help manage your condition at home:
Regular Exercise: Low-impact activities like yoga or swimming can strengthen the pelvic muscles and improve flexibility, helping to reduce pain.
Relaxation Techniques: Mindfulness meditation, deep breathing exercises, and other relaxation techniques can help reduce stress, which may, in turn, decrease pain levels.
Healthy Diet: Eating a balanced diet that avoids triggers like caffeine, alcohol, and spicy foods can help alleviate symptoms of IBS and other gastrointestinal conditions that contribute to pelvic pain.
Pelvic Floor Exercises: Strengthening the pelvic floor muscles with exercises can help alleviate pain, particularly in those with pelvic floor dysfunction.
Conclusion: Take Control of Your Pelvic Pain Today
Chronic pelvic pain can have a profound impact on your quality of life, but you don’t have to live with the pain. At Mitigate Pain Clinic, our team of specialists is committed to helping you find relief through advanced interventional pain management techniques. We work tirelessly to identify the underlying cause of your pain and develop a personalized treatment plan to help you regain control of your life.
If you or a loved one is suffering from chronic pelvic pain, contact Mitigate Pain Clinic today to schedule a consultation and take the first step toward a pain-free future.
Frequently Asked Questions (FAQs)
Our Treatments
- Joint Pain
- Back Pain
- Sciatica Pain
- Neck Pain
- Hand Pain
- Shoulder Pain
- Foot & Ankle Pain
- Limb Pain
- CRPS Pain
- Cancer Pain
- Headache
- Hyperhidrosis
- Herpes Zoster Pain
- Chronic Pelvic Pain
- Scar Tenderness
- Postherpetic Neuralgia
- Trigeminal Neuralgia
- Peripheral Neuralgia
- Chronic Vascular Pain
- Generalised Body Pain
- Chronic Injury Pain
- Failed Back Surgery Syndrome
- Chronic Post Surgical Pain
- Other Painful Conditions
- Slipped DISC / PIVD